The Healthcare Breakdown No. 045 - Breaking down the theory of relativity in how much work doctors actually do
Brought to you by Forward Slash / Health: it's super cool to be a clinician and entrepreneur
What we’re breaking down: How physicians get that paper, (hint it’s the wRVU)
Why it matters: A lotta docs, the employed ones, get paid for productivity… ain’t that a b?
Read time: Less time than it took me to get to the airport on Wednesday (8 minutes for real though)
This episode is brought to you by!
Forward Slash / Health works with clinicians to launch and accelerate their businesses, whether that be a private practice or healthcare startup. Forward Slash / Health specializes in compliance, financial optimization, strategic planning, and operations management. And being awesome.
I added that last part. They don’t know about it. But they are, awesome.
Currently taking limited applications for new clients. Follow the link below to learn more and apply!
I swear, we’re starting soon, but if you noticed that giant billboard right up there above your current reading line of sight, The Healthcare Breakdown is now taking sponsors. It’s just little ole me rockin this thing out and I refuse to ever make this publication paid. Hence the sponsors.
We’ll keep it fun with only cool people who can add to the hilarity. If you’re interested in sponsoring and getting your own billboard, clicky click below and let me know!
And onto the show!
I am quite sure that when Albert Einstein was coming up with the theory of relativity, he was definitely thinking about the relative value that doctors provide when treating their patients.
It’s no wonder then, as one can imagine, that we both judge and incentivize doctors based on the relative value they produce.
Ok, homie, what am I talking about…
I am talking about RVUs or Relative Value Units. RVUs are a measure by which Medicare, in its infinite wisdom, determines how much to pay a doctor for the work she performs.
Come, walk with me down memory lane. Way back in the days of too much hair spray, Lycra, and hot pink pants (the 80’s), doctors were paid by Medicare based on Customary, Prevailing, and Reasonable charges. Essentially, we used to trust doctors to set their own rates and Medicare, after a tiny bit of voodoo, would pay them.
But we all know doctors are not to be trusted and the tables began to turn as rates began to rise. Imagine that, prices for things increasing. Never happens anywhere else in the service industry.
While rates rose the cost of procedures began to fall. Naturally, since these medical services were meant to be compensated based on cost and not value, the powers that be opted for the adoption of the Resource-Based Relative Value Scale.
At least they left the word “Value” in there to make us all feel warm and fuzzy. This represented a fundamental shift to payments based on the cost of providing care, rather than self-directed pricing and arguably value. That’s a whole different discussion though.
Back to the action. So, in 1992, 5 years before the peak of our society, Medicare began compensating physicians based on RVUs.
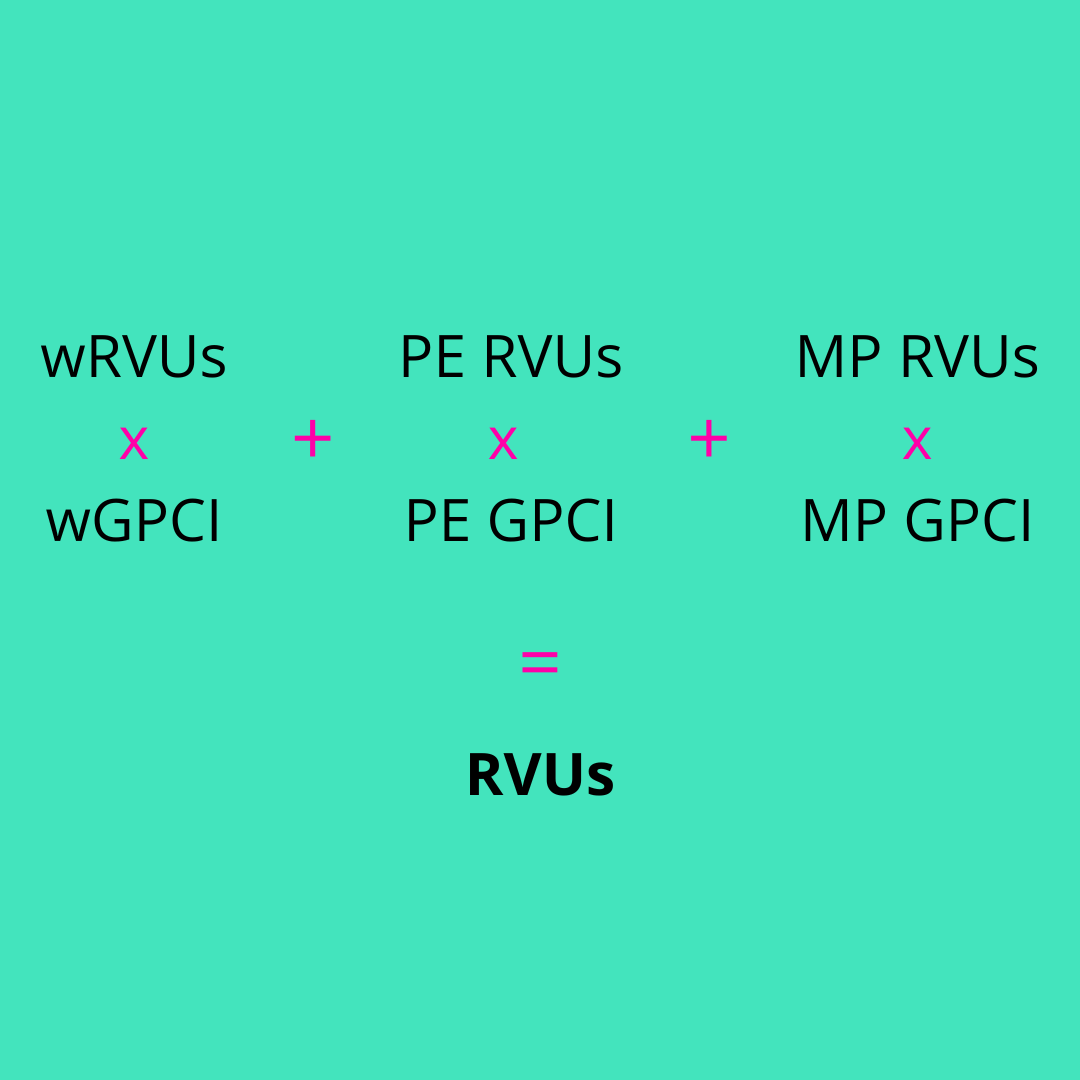
Here’s how RVUs are calculated:
This is the short version. Here’s what it all means:
wRVU = Work RVU. In other words the amount of work, time and effort, a physician directly does for a certain procedure. As you can imagine a primary care doc seeing a patients is far less of an wRVU than a neurosurgeon removing a tumor. But don’t worry, we’ll get there.
PE RVU = Practice expense. This is the additional cost that a practice incurs to perform the work. Admin, overhead, supplies and all that.
MP or PLI RVU = Malpractice or professional liability. The cost to CYA. That’s another highly technical acronym that approximately means cover your tush.
And who comes up with all this you ask? Well the RUC of course. The Relative Value Scale Update Committee. More or less a secret society of well to do, high powered, occasionally consultant backed, physicians who determine wRVUs. It’s a topic for another time but there is a whole lot of politics, power, and money going on behind the scenes of the RUC. Like that move The Skulls. Miss ya Paul.
Then we get real fancy pantsy and add Geographic Practice Cost Indices (GPCI). Ya know, cost of living type deal. It’s more expensive to rent office space in New York City than it is in Topeka, Kansas. You also work harder in New York.
Just kidding. But a sandwich there cost at least .065 wRVUs more.
One more thing for the icing on the cake. We clearly need to take into account facility location. To do that we add POS codes. POS stands for Place Of Service, get your head out of the gutter.
You have essentially two buckets, the facility and the non-facility.
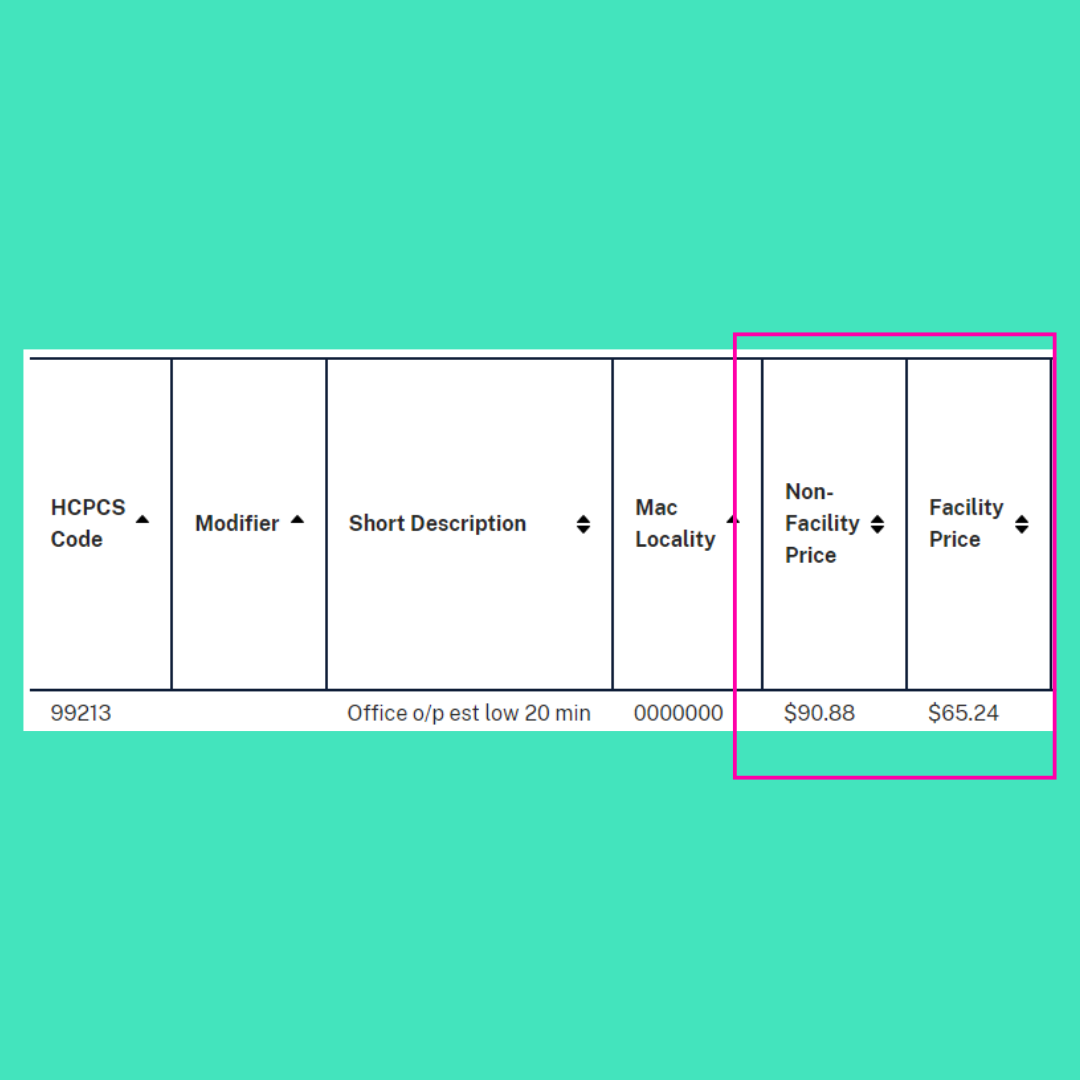
This becomes slightly counterintuitive. As you can see below, for this code, everyone’s favorite E/M (evaluation and management) 99213, the facility price is lower than the non-facility price.
Why you ask?
Well, because everything the government and healthcare does is super simple. So much so that we are currently talking about the physician fee schedule. Not the Outpatient Prospective Payment System or the Inpatient Prospective Payment System. We are also not talking about DRGs, (diagnosis related groups).
Omg, it just makes you want another mimosa. In fact, be right back.
So, the difference is because under this particular fee schedule, the Physician Fee Schedule, we’re just talking what the doc gets paid. In a non-facility we are assuming that is the doctors practice and so the price takes into account that care setting. It adds more to cover costs associated with running the practice.
The facility price assumes a hospital or other larger facility that is eligible to bill a facility fee. Which, it of course does and really needs to. But it shockingly ends up being a huge chunk of the reimbursement. Because surprise, surprise, hospitals have a lot of overhead to keep that waterfall on in the lobby 24/7.
To finally arrive at these reimbursement rates we need to apply the Conversion Factor (CF), which lucky for us and everyone else, CMS has been lowering year after year.
Just kidding. Talk about a mechanism to further choke independent physician practices. Ever hear of inflation? Anyways, back to this confusing entanglement.
Here’s the calculation. This is an easy one.
RVU * CF = Price
We are now left with a CPT reimbursement price or rate that is predicated on the illustrious RVU, driven by the wRVU, which is determined by the mysterious RUC.
And here is the punch line. All hospitals and large group practices are trying to make the most amount of money and grow. To do that they need to bill more. To do that, they incentivize their doctors based on their productivity.
To do this, they write contracts that ties compensation to RVU production. And as we have seen, the wRVU is the basis.
So if you’re an attractive 37 year old general surgeon that I grew up with, you may have a contract that requires you to hit 6,000 wRVUs each year to hit your salary target. Anything above that is gravy and you’re looking at bonuses.
You know what we call that in the sales world? A commission and bonus structure.
Funny thing when your doctors, your surgeons are paid based on production and incentivized to do more. Because really, shouldn’t we be trying to avoid surgery and procedures?
Two more things to really ruin your day.
First on the surgery front.
Second on the primary care front.
Let’s go back to McDreamy for a moment and consider a procedure he does on the regular. The cholecystectomy or otherwise known as, removal of the gallbladder. Seriously, if you aren’t using yours, let me know. He loves taking those things out.
There are two ways to snake that thing. First, tried and true, cut ya wide open and snip it out.
Here’s the wRVU situation for that:
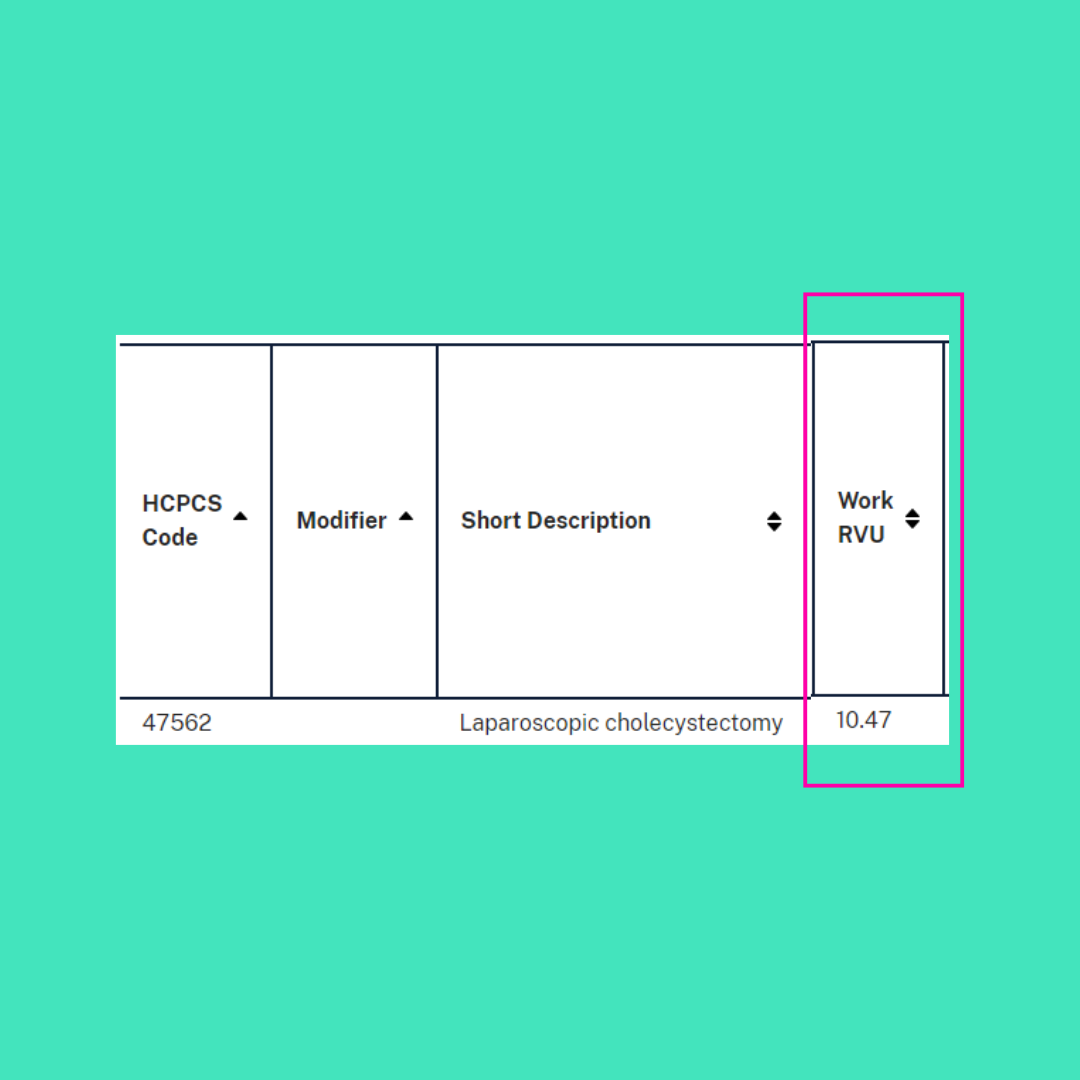
The second way with minimally invasive, the laparoscopic way. In his case with a swanky robot named Xi. Here’s the wRVU situation for that:
Guess which one is easier (according to him and other surgeons I have spoken with) with longer recovery times and higher risk for infection. Yup, the one that gets higher RVUs.
That means the hospital makes less and the doctor needs to do more to hit their comp targets if they choose the better procedure type.
Luckily McDreamy is McDecent and does the right thing. But it does bring into harsh perspective what exactly is going on with these incentives and how our system is designed.
Cool, that sucked, but let’s also look at one more sucky thing. The wRVU of the primary care doctor.
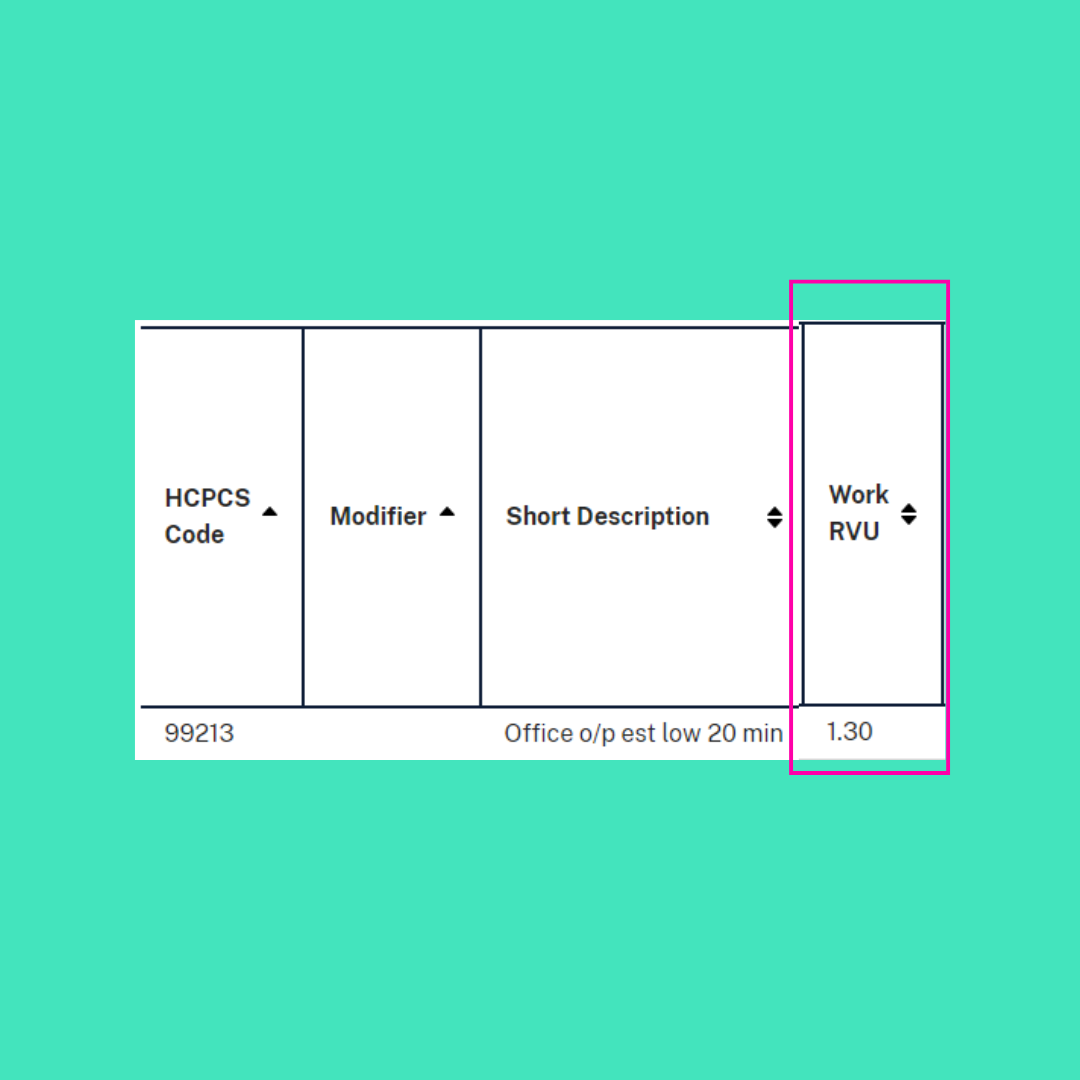
Let’s go back to the 99213.
wRVU of 1.3.
Compared to an open gallbladder theft wRVU of 17.48.
Now look, I’m not trying to rock an apples-to-apples comparison of cutting someone open and removing their organs without killing them to sitting and listening to me complain about not wanting to exercise and asking question after question about just how much red meat I can eat while still wanting my cholesterol to come down.
But there is a fundamental issue when we are reliant on primary care to focus on prevention, coordinate so much care, and spend tons of hours charting, none of which falls into any RVU category, and then tie their salary to productivity which we have set to an incredibly low rate. Not to mention the fact that it takes an incredible amount of broad knowledge and expertise, which in itself is challenging to leverage and apply to high level patient care. Our primary care docs aren’t working any less, but it’s clear that their work is, let’s just say valued differently.
And while I am on riding this rant wave, the traditional fee-for-service, production payments make no sense in the primary care setting. And before you come at me with Value-Based Care, sure, Oak Street Health may be making money on risk-based contracts, but guess what? Their docs are still expected to see a certain number of patients and are paid on productivity not savings. That’s an organizational metric.
One last blather… yes, also quotas for primary care docs are set lower to match the low wRVU. But we can look at the concurrent reimbursement for the CPT and the earning potential of our primary care docs versus the procedural based specialists and see the significant gaps.
Fairly clear that we undervalue primary care and spend a lot on procedural specialty.
I love my specialist homies. Need em. They’re great. Love you all. But I would hazard a guess that they might appreciate a little more breathing room if they didn’t have cutting quotas and got the full space and support to practice how they wanted to without hitting RVU metrics.
Maybe I’m wrong. Maybe they love having productivity quotas. It all still feels pretty misaligned to me though.
Here's the TL;DR…
Docs are paid largely on commission.
The RVU was well intentioned (isn’t everything), but it drives misaligned incentives.
Primary care in undervalued, relatively and actually.
Healthcare is a real bummer sometimes.
Mimosas are always on the menu.
I shouldn’t be given authority over a TL;DR section.
I love you.
Until next time.




Btw I have no problem with surgeons and other highly trained specialists making more than me as a psychiatrist- they deserve it! But you are correct to point out how misaligned Medicare and insurance payment structure can be. How confident would you feel after 10 min with your psychiatrist that they are able to adequately assess your presentation, make a tx recommendation, provide pt education and informed consent? Let alone coordinate with your PCP or therapist god forbid. Not gonna happen when we are chasing reimbursement in an environment where payment is going DOWN. Forget keeping up with inflation. Can anyone say “payment reform now please”?
You always manage to bring clarity to the most complex financial issues! Thank you for your #thoughtleadership! Docs are paid largely on commission.
The RVU was well intentioned (isn’t everything), but it drives misaligned incentives.
Primary care in undervalued, relatively and actually.