The Healthcare Breakdown No. 047 - Breaking down a series kickoff on PBMs!! Part I: What the devil is a devil, I mean PBM?
Brought to you by Forward Slash / Health
What we’re breaking down: Pharmacy Benefits Managers (PBMs)
Why it matters: PBMs control access to and prices of drugs
Read time: The time it takes to checkout at the pharmacy counter when you also bought groceries (please don’t be that person by the way) (7 minutes for real though)
We’re doing a series!!!! Ahhhh. I haven’t been this excited since Taylor announced a double album for TTPD. IYKYK.
Non-healthcare related acronyms aside, let’s talk about PBMs! Otherwise known as Pharmacy Benefits Managers. Here’s how this is gonna go.
You are living in Part I right now. The background on PBMs and how they work.
Part II will cover the ecosystem of pharmacy and bring in some of the other players.
Part III will show you the money games PBMs play.
Part IV is gonna dive into the real world of pharmacy and how this all plays out. We’ll circle back to GoodRx, look at real examples of what’s happening out there, talk about vertical integration, intercompany eliminations, and all that hoopla.
There will probably be a Part V, but that depends on John. You know who you are.
I also reserve the right to completely change the order of everything above, or retire early and become a woodworker living in Ireland for no apparent reason.
On with the show! After a word of course from our illustrious sponsor:
This episode is brought to you by Forward Slash / Health
We know what you're thinking, "these hot-pink-shoelace wearing folks are going to come in here and tell me all the things I've been doing wrong, pat me on the head, and tell me they will handle the business so I can 'focus on my patients."'
We get it, but that's not how we do things at Forward Slash / Health. This is your business. We are here to support you and your organization. We are a part of your team, not the other way around.
You will never be absent from the decision making process. We tailor our approach so you can be involved as much or as little as you want.
Back to the action that still hasn’t started yet. What in the world IS a PBM?
When medication started becoming this fancy designer thing, insurance companies started covering it in the 60’s. Naturally, patients and drug companies were into the idea leading to increased utilization and cost. As a results, PBMs emerged to help manage drug benefits.
Originally, the intention was to simply be insurance for drugs. They (the PBM) would pay the pharmacy the Usual and Customary (U&C) price for a drug. It was basically the cash price a person would otherwise pay. Just like the insurance company paid for medical services. Simpler times.
Over time, PBMs began growing in size and scope, operating in the exact same ways as insurance companies, only focused on drugs. They built their own networks and charged their own rates based on growing market power.
Man, I love the smell of capitalism in the morning.
I will spare you all the acquisitions and spinouts that got us to the PBM landscape we have today. Here’s what you really need to know:
There are 3 PBMs that control 80% of the market. They’re the game.
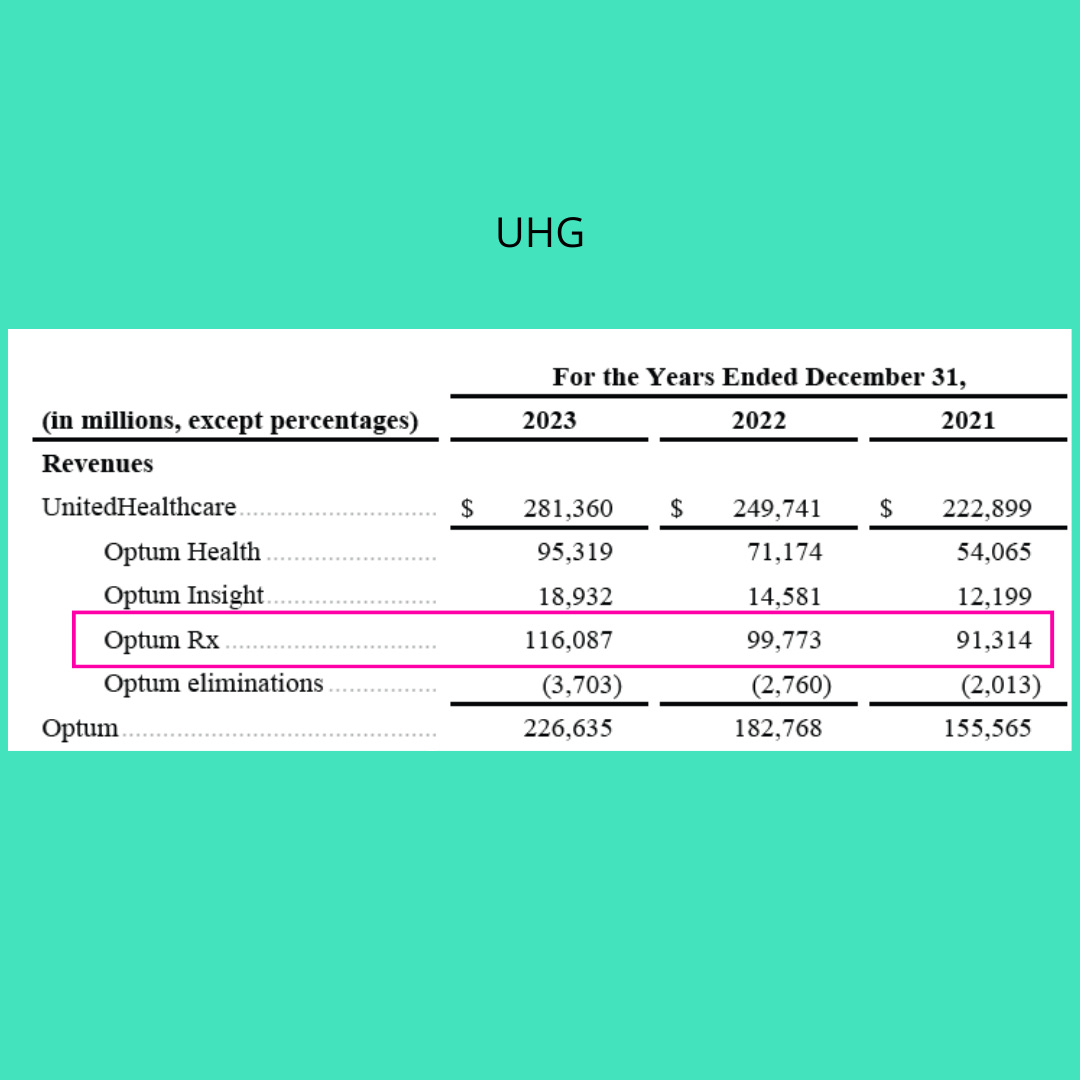
OptumRx (UHG)
Caremark (CVS)
Express Scripts (Cigna)
I wonder if Cigna feels left out for not having a sweet three letter abbreviation?
You will notice that these three ever so large PBMs are owned by three ever so large insurance companies. I also love the smell of vertical integration in the morning.
And because you didn’t ask, we just have to see how much money all these companies made last year. Just gotta. It’s half the reason you’re here:
Wow… That’s a lotta cheddar.
A note on CVS. Its Health Services Segment includes more than just Caremark. It includes the likes of Oak Street Health. But since that’s in the pooper, it’s safe to say that Caremark is the vast majority of this segment.
Now that we know the major players we can look at the most confusing diagram on the planet.
Here you go…
That my friends is the PBM/pharmacy ecosystem.
I put the PBM in the middle, because they are the ones orchestrating all the madness out there. Deciding what drugs are covered. Deciding what qualifies someone to follow their doctor’s orders and take a drug. Deciding how much everyone, including themselves, get paid. And deciding how much we, the patients, will pay.
Ok, you have seen the super confusing diagram. I am going to walk through it in the only way I know how. Through rambling and a grammatically poor semi-stream of consciousness.
Sidebar: while we walk through this, just pretend that the insurance companies don’t own the PBMs. Imagine them as separate entities. It’s easier to visualize.
So, the plan sponsor (your employer) signs up for a health plan or makes a health plan. Or pays a broker to do everything for them and gets a bad deal. That’s a whole other story. If they are self-funded they will also pick a PBM. If not, they’ll just use the insurer’s.
Crap, I already messed up. They were supposed to be separate. Ignore me. But keep listening.
So, the health plan now has an insurance carrier and a PBM. One for the drugs, one for the doctors.
Now, the PBM goes out and talks to the drug manufacturers. Says, hey, I’m going to need these drugs on these tiers and here is how much money I want in exchange for the honor of including them on my formulary. I would also like this much money if I sell a certain amount of these awesome drugs. And probably not the last thing, but I would also like money back for selling certain drugs or selling enough of certain drugs.
Cool, check, we have the covered drugs on the plan. Now, the PBM goes to all the pharmacies to flex. Basically they do the same thing insurance carriers do.
They say something like… Hey, I have like a billion covered lives, if you want them in your pharmacy, you will be part of my network and take my drug coverage. I am going to pay you x for y and there is about zero you can do about it. Oh, I will also come back from time to time and take back money if you don’t hit certain metrics that I totally make up. It’s awesome. We call it a claw back. Cool right? Right on, later gator.
The PBM also tells the pharmacy what to charge you, the poor unsuspecting patient. So whenever you roll to Walgreen’s and they tell you your generic statin will cost $93.66, you have the PBM to thank.
Now the PBM hikes back to the plan and says, hey, I got it all worked out. Don’t worry, I’ll cut you in on the hustle and you won’t have to lift a finger. In fact, the less you ask, the better. Smooches.
The dialogues have been slightly changed, but that’s about the gist.
The PBM then sits back and collects on all the obfuscation.
And because he PBM is just a fee taker, their incentive is to drive down the reimbursement to the pharmacy but drive up the cost everywhere else in the chain. That eventually hits patients’ wallets.
We’ll get into this more in part número dos. For now, the key here is that PBMs are out there taking fees, rebates, and slices of everyone’s key lime pie.
Now, for that practical stuff I promised.
Fun fact, most drugs, especially generics are super duper cheap. We’re talking like 2 cents per pill. And as a patient, nothing stops you from asking what the cash price or the lowest price a pharmacy can charge you.
And as a doctor, there is not much stopping you from dispensing common generic medications from your office. Ok, maybe there are some big caveats, but states do allow physicians to dispense directly from their offices. You can focus on low-cost generics, for instance, and charge cash rates in certain circumstances. You can also focus on commonly non-covered drugs. Boom, saved a trip, probably saved money, and kept a closer eye on your patient.
Now, none of what I just said is take it to the bank type of advice, but it’s certainly worth exploring. With some compliance experts for sure!
Sooooo, there you have it. Now you know what PBMs do. Well at least the “purpose” they are supposed to serve.
Next time, while you sip sangria we’ll jump into that super fun ecosystem image to see what in the world is going on.
In a while crocodile.






3 PBM’s in the U.S. control 80+% of market, an incredible oligopoly that hammers individual patients.
ThanksPreston, for another great article adding clarity to a system that seems designed to obfuscate. One has to ask, "Why is this like this, and how did it get started?" Looking forward to your answers in the subsequent posts.