The Healthcare Breakdown No. 058 - Breaking down Charge Masters of the Universe
Brought to you by Grayskull
What we’re breaking down: What’s the deal with chargemasters, charges, adjustments, and why all the numbers in healthcare seem to be made up
Why it matters: Understanding this new age math can help private practices stay that way and patients/employers understand what they are really paying for
Read time: As long as it took you to realize He-Man and Ivan Drago are the same guy (7 minutes for real though)
And now, a word from our illustrious sponsor:
Forward Slash / Health works for physicians. Yes, they work FOR Physicians… to escape the unrelenting crush of administrative burden, run financially successful practices so you can take your significant other on Disney cruises whenever they want, and stay totally independent after you let the private equity company fly you somewhere fancy to eat caviar and drink champagne on their dime just to say politely but not too politely…. ummmmmm pass.
*Unnecessarily silly language added for style and because that’s how I roll. They are much less silly, but still, the right amount.
Give ‘em a call!
I totally missed you too.
Now that we have the sappy stuff out of the way, let’s jump into math that makes less sense than common core math. IYKYK. What’s up parents.
That’s right, today, we are talking about charges, chargemasters, and how in the world your bill went from $22,000 down to $1,700.
Ya, you wish.
On the flip side, for all my doctor fraynds, it’s also key to your practice. Because while you are charging $238, they ain’t paying you that. But then again, if you charge less, you may be leaving money on the table.
Let’s start with the patient perspective, because we’ve all been there.
Here’s a bill from the internets:
Thank you Kaiser Bill of the Month Club. This poor soul went for a colonoscopy and got charged for two. Classic.
But what I want to point out is the this top section here:
We’ve all seen it. We don’t love it. We don’t know what it means, or why it exists.
But I’ll tell you.
The what it means part:
First up we have “Charges.” This one is going to come up a lot and it’s common from all the perspectives and settings. This is what the hospital, the doctor, the practice, the whatever, charges. This is the same charge for everyone. It can be for a private plan or Medicare. It can be for you or me. Doesn’t matter, this is the “price” set by the care provider.
But they know, now you know, we all know this isn’t what they will or anticipate being paid.
Silly right? It gets better.
Next column, you see, “Adjustments/Ins Payment.” Sometimes this is broken out into two columns, but why waste paper space or make things easier to understand. This is healthcare dang it.
This column shows both what has been adjusted and what insurance has paid. Since that makes no sense, here’s what that meaning means:
A doctor (you, if you are a doctor) contracts with an insurance company. I would say that you both agree to what they are going to pay you for certain services, but we all know that’s not entirely true…
Anyways, you have a contract with the insurance company for an “Allowed Amount.” That’s the contracted rate. Another column would then show what the plan or the “payor,” paid.
And if you decoupled the “Adjustments/Ins Payment” column you would also see the adjustments made. That would simply be the difference between the charges and the allowed amount. Good old subtraction.
To be fair, from the payor perspective it does make sense to lay it out this way. When they do, it shows why you have insurance in the first place. If not, look at those charges! You would be on the hook for all of it without those nights in shining armor. Or in He-Man’s case, shining speedo armor thing.
This is the game.
Blue Cross Blue Shield actually has a nice little example on one of its 12,000 websites. Here’s the image:
To bring it all together, here’s what the the first bill and the above Explanation of Benefits tells you:
What the “price” of the service is
The difference between the charges and the allowed amount, or the adjustments made
How much the insurance company is contracted to pay (sometimes)
Shweet. Then you can tell how much you are on the hook for.
Not too shabby. Why do I even write this thing (I constantly ask myself), you could have totally figured that out.
But wait, there’s more!
Why, good madam, do we even have these wily charges? The fanciful things that everyone knows no one is going to pay?
I will explain by asking you two questions….
Does Africa have more or less than 10 countries?
How many?
Don’t peak at the answer!
It’s 54.
How many did you guess (unless you are a geography wizard and know)?
What just happened to you was anchoring. Anchoring is a point of reference that you subconsciously set based on some potentially unrelated or arbitrary input. The first question anchored a low number in you mind. When you do this, the majority of people will guess a lower number than 54.
If I had asked does it have more or less than 60, you probably would have been closer and guessed a higher number.
Weeeee psychology!
Soooo…. When you see this:
(And who said that L&D was a money loser…)
You know this is anchoring in action.
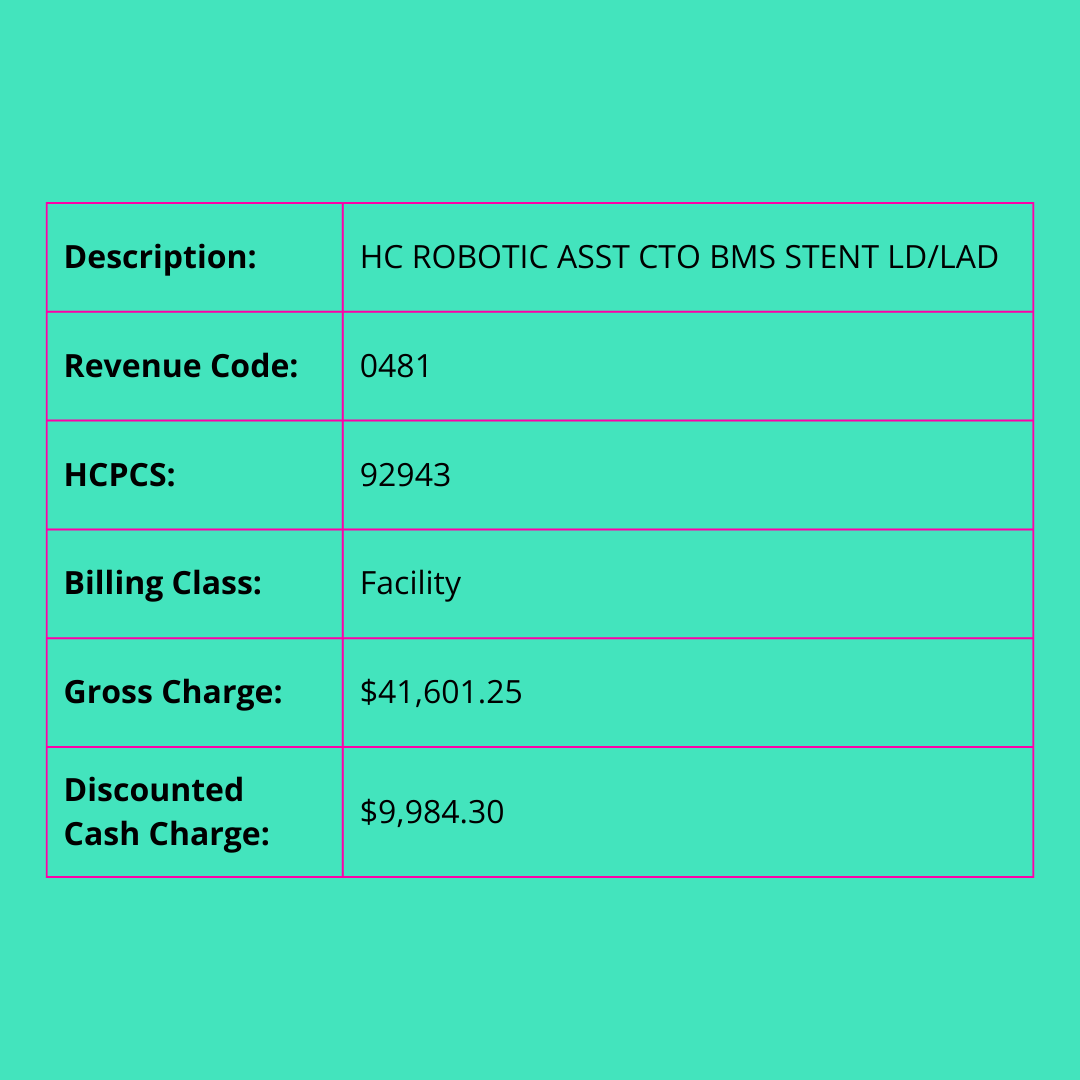
This too:
I had to make my own chart, because chargemasters ain’t pretty.
Not too shabby for a gross charge. Just a little 317% mark up over the discounted cash charge.
And anyone’s guess what private insurers are reimbursing this for.
If I had more time and patience, I would have calculated the Medicare rate, but as reliably as He-Man yelling that he has the power unnecessarily, like we know guy, we know… it is a huge pain in the tuchas to get all the info together from CMS.
Honestly, it’s no wonder that hospitals have to spend so much money and time on their billing departments. It’s not an easy game.
They do make it easy to look up physician fees though. Which is mighty nice of them.
Here’s what a physician is going to make from Medicare for the procedure:
That’s sweet.
Who is it that’s driving up healthcare costs again?
Anyways, back to this code provided courtesy of Wellstar. It provides a glimpse into the complexity and the madness of charges, adjustments, and all the morass.
But back to the anchoring for a moment. Two reasons charges are silly/not silly. They serve as a foundation for negotiation with these alleged payors. Anchor high as a starting point.
Additionally, in every contract the language stipulates that a payor will pay the lesser of charges.
That means that if your contracted rate is $125 but your charges are only $115, they gonna pay you $115.
I mean I would.
This brings me to my next point.
This one is for you my private, independent practice homies.
Get your charges right. There is some art and some compliance science to it. But what you definitely need to know is that your charges need to be higher than your contracted rates. If not, you will get the lesser of the two.
Silly game? Yes. Game you have to play? Yes. So know the rules.
And I agree with everyone reading this that’s like, “well it’s the insurance companies, and opt out, and Bucky Fuller, and other fist shaking shouldas.”
But we are here, right now. And for a physician working to remain independent, care for their patients, and stay in business, this is how it works.
Change? Yes, please.
We can do both at the same time.
Ok, I think that’s enough high horsery for today.
I still love you.








Great to have you back and with a wonderful sponsor no less.
although it was a wonderfully laid out (as always) I believe you missed an important aspect. The delta between the billed charges and the paid charges also becomes a “loss” on the hospitals books (especially those wonderful Not-For_Profit ones) and helps to explain how they can consistently lose money on every case that have drained building additions and pay their executive staff millions in pay and bonuses for money well lost (I’m sorry a job well done)