The Healthcare Breakdown No. 060 - Breaking down those sweet 340B discounts and how much patients aren’t benefiting
Brought to you by Jessie
What we’re breaking down: That one program you hear a lot about that seems great but when you really peel back the onion you realize it’s really just another way for large healthcare companies to get richer while we all, don’t – ya, I know that could be any program in healthcare, but today, it’s 340B baby!
Why it matters: This program allows the rich to get richer while the poor stay that way
Read time: As long as it took Sanka to win his 7th push car championship (6 minutes for real though)
Let’s be real for a minute. If you really want to go deep and get the real deal look at the 340B program, put down this newspaper and head to Drug Channels. Adam Fein is THE authority on drugs. Yes, even more than Walter White. Nicer too.
And since he’s smarter and more attractive than me, many of the graphics you will see in this episode come straight from the illustrious Adam Fein himself.
Ok, if you stayed to hear my take, the simpleton’s version, let’s get right to it.
Let’s start with the obvious question:
But Preston, how can it be bad for poor old rural hospitals to buy drugs at a discount from big old mean drug makers?
Well, sweet little Jason, I will tell you. But first! What even is 340B?
It’s a no longer little program that went into effect in 1992. The year before the perfect retelling of the triumphant story of the Jamaican bobsled team that forever changed the world of bobsledding, Disney magic, and lucky eggs. The program allows “covered entities” the ability to purchase outpatient drugs at a steep discount from drug manufacturers.
Covered entities used to include a very limited number of facility types that you might expect such as Ryan White centers, Federally Qualified Health Centers, tiny little, baby little rural community hospitals, and the like. Nowadays, thanks to everyone’s favorite punching bag, the ACA, the qualifications for a covered entity has greatly expanded. The darling of that expansion is the so-called Disproportionate Share Hospital (DSH).
A DSH like metro Atlanta’s very own, Wellstar. That same one that runs a $100M venture fund and bought a hospital for $800M right after closing one of two of Atlanta’s only level one trauma centers that happened to serve a low-income community.
No, no, I’m not bitter.
But you probably can start to see the issues.
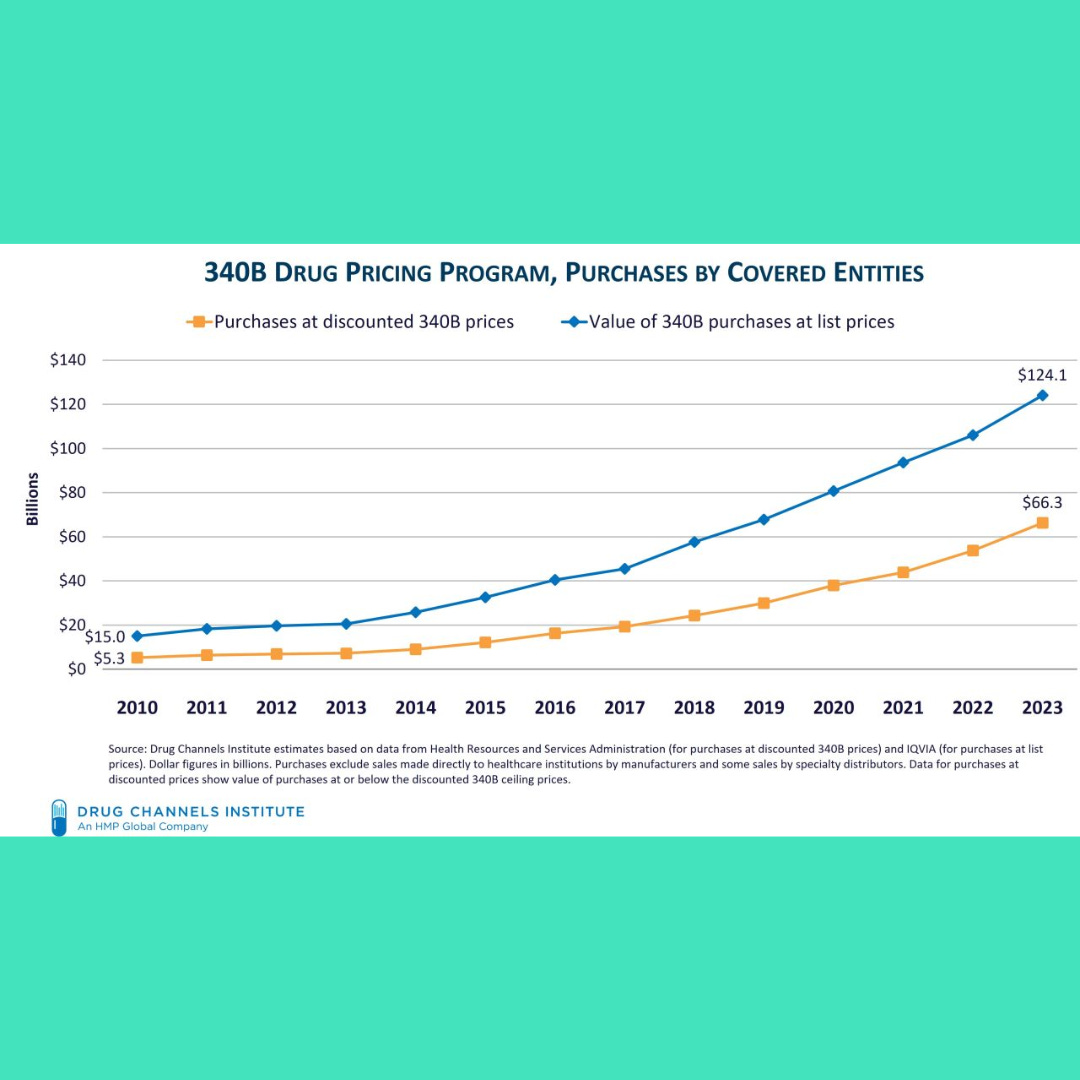
And here how the program has grown in dollars, both program value and purchase price:
That’s a lotta cheese. And in fact, is now the second largest drug program right behind Medicare Part D. Ya, the big dog.
So, in 2023 covered entities purchased $124B worth of drugs for $66B.
Back to the original question of why is it so bad for hospital, even those really rich ones, to buy drugs at a discount? Especially since the drug companies can afford it? Well, sit down here on grandpa’s knee and let me tell you how capitalism works.
If my profit margin is eroded by say, mandated discounts and loopholes in a well intentioned but poorly governed program, that allows organizations like Ascension, Cleveland Clinic, and NYU Langone (Ya, that hospital that made $1B in cash and burned $8M on a Super Bowl commercial that wasn’t even funny) to buy drugs at half the price, then I’m just gonna go ahead and raise the price.
Don’t start telling me I’m wrong yet, you well educated lot. Drug companies do have to provide rebates if they raise the price of covered drugs more than inflation. Good thing drug companies don’t just make one drug now isn’t it. Also good thing that there are lots of channels in which to sell drugs.
We’re talking about the ripple effects to the whole system here.
This is the basics. When you are trying to maximize sales and profits, you look at your mix and raise prices where you can to offset lower margin drugs.
Yes, the expansion and rise of 340B utilization definitely has helped to propel the rise of drug costs.
But it’s not just manufacturers. I know everyone likes to pick on them, but don’t forget about the darling PBMs. And those lovely covered entities too.
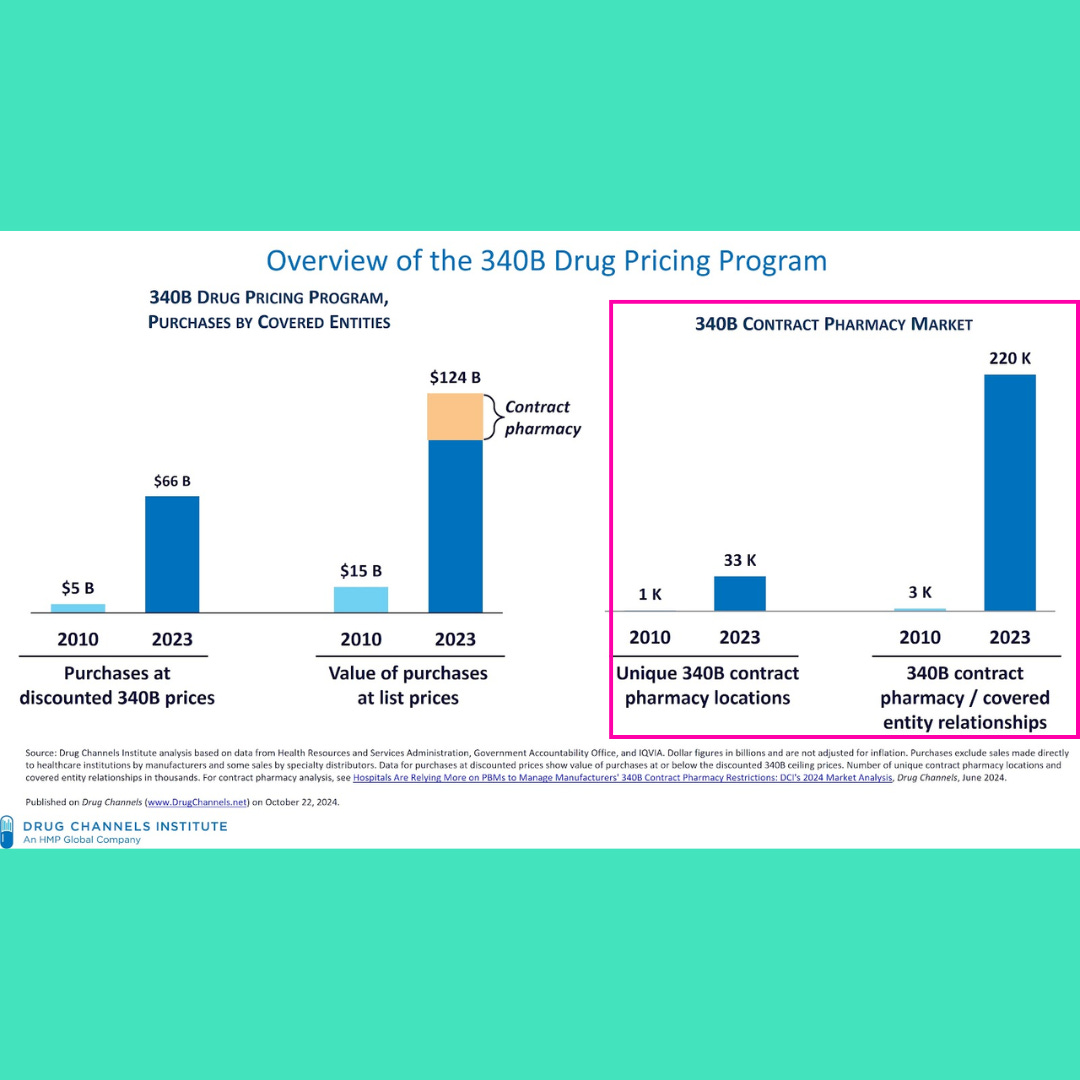
So, around the time of the program’s expansion, the government also told hospitals that they were allowed to contract with pharmacies to dispense 340B eligible drugs. That meant that the hospital didn’t even need to touch the drug. It could just send a patient on their merry way to Walgreens or CVS to pick up their covered drug.
Or better yet, they could do a mail order script. Love those. And guess who manages all this fun?
Ya, Pharmacy Benefits Managers. And when hospitals were allowed to use contract pharmacies instead of in-house, the number of contract pharmacies exploded to over 30,000. Not to mention the over 200,000 contractual relationships between all of these pharmacies and covered entities.
OK, I know we are having more fun than a Jamaican bobsled team line dancing in Canada.
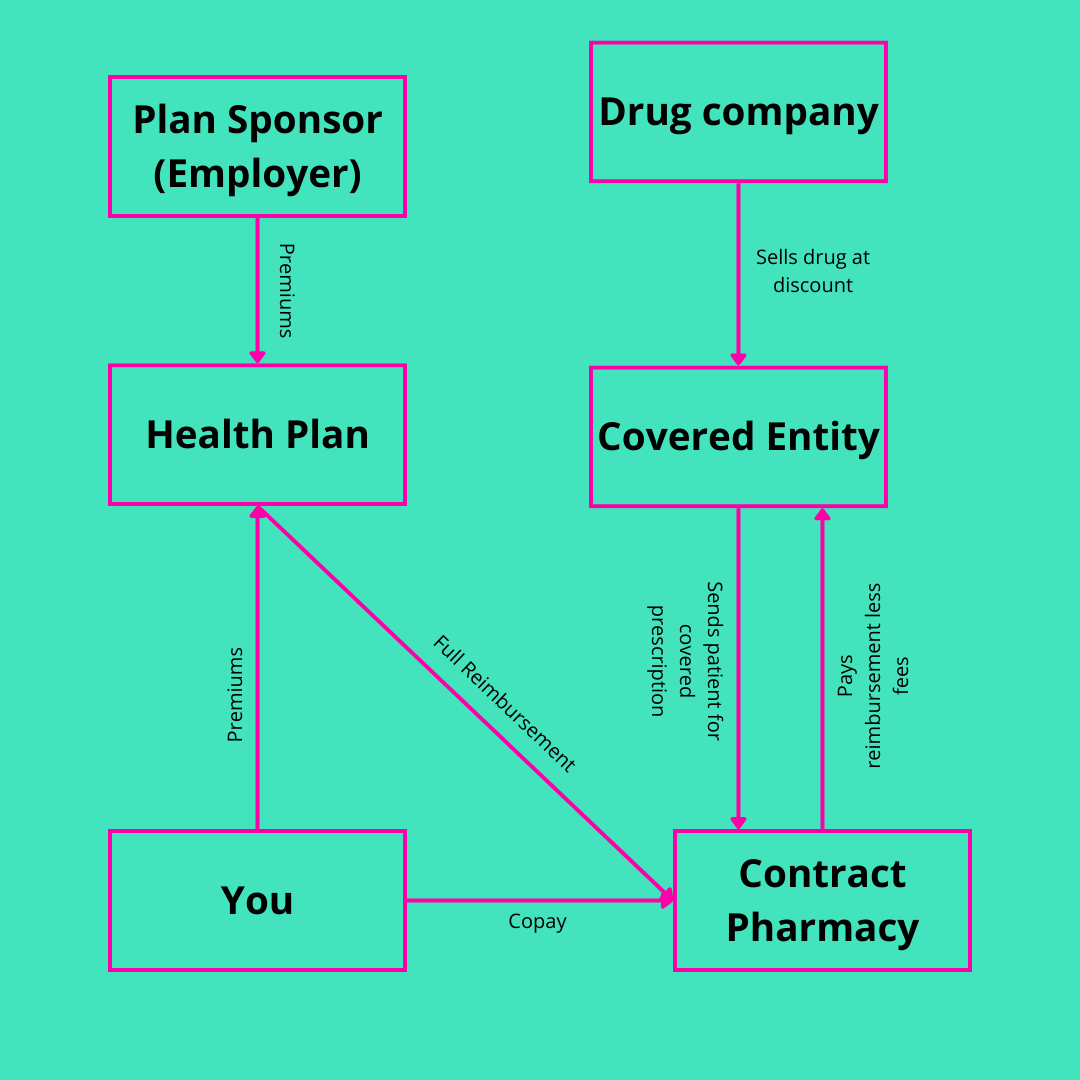
Here is how things flow when a patient who is 340B eligible gets their meds:
A simplified version of course. There are a couple more middleman missing as you might imagine, but this is the gist. What’s wild is the hospital doesn’t even need to touch the drug. Oh, and there’s more…
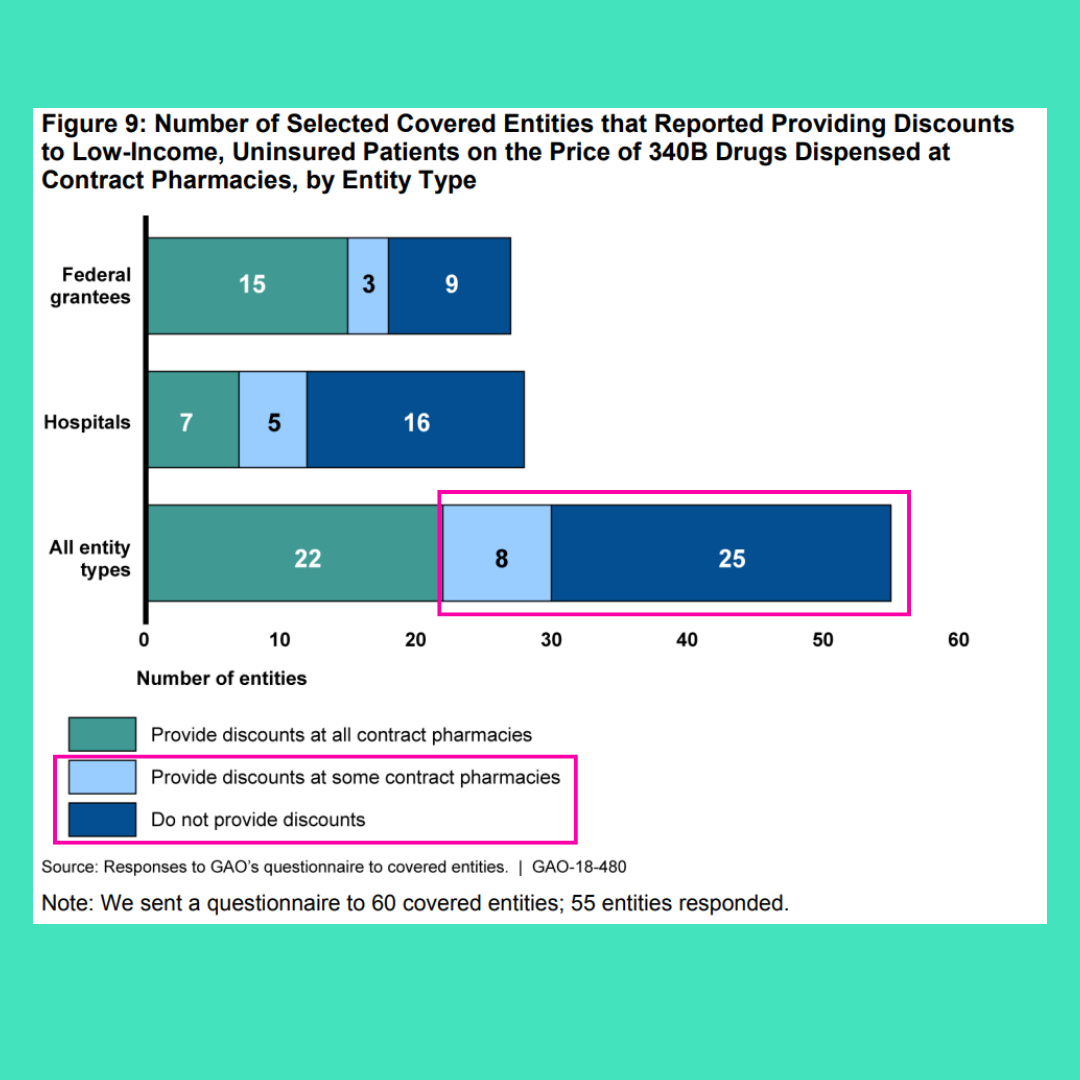
And again you are thinking, so what Preston pants? The patient must be getting some of that savings, right… right????
Ya, sure all you healthcare junkies. Sometimes.
Like this many times:
Ya, less than half the time.
Fun right.
What does this mean? This means that hospitals are pocketing profits and not passing along the savings to their patients. And not just the hospitals. The contract pharmacies too.
You know Optum isn’t leaving someone else’s money on the table.
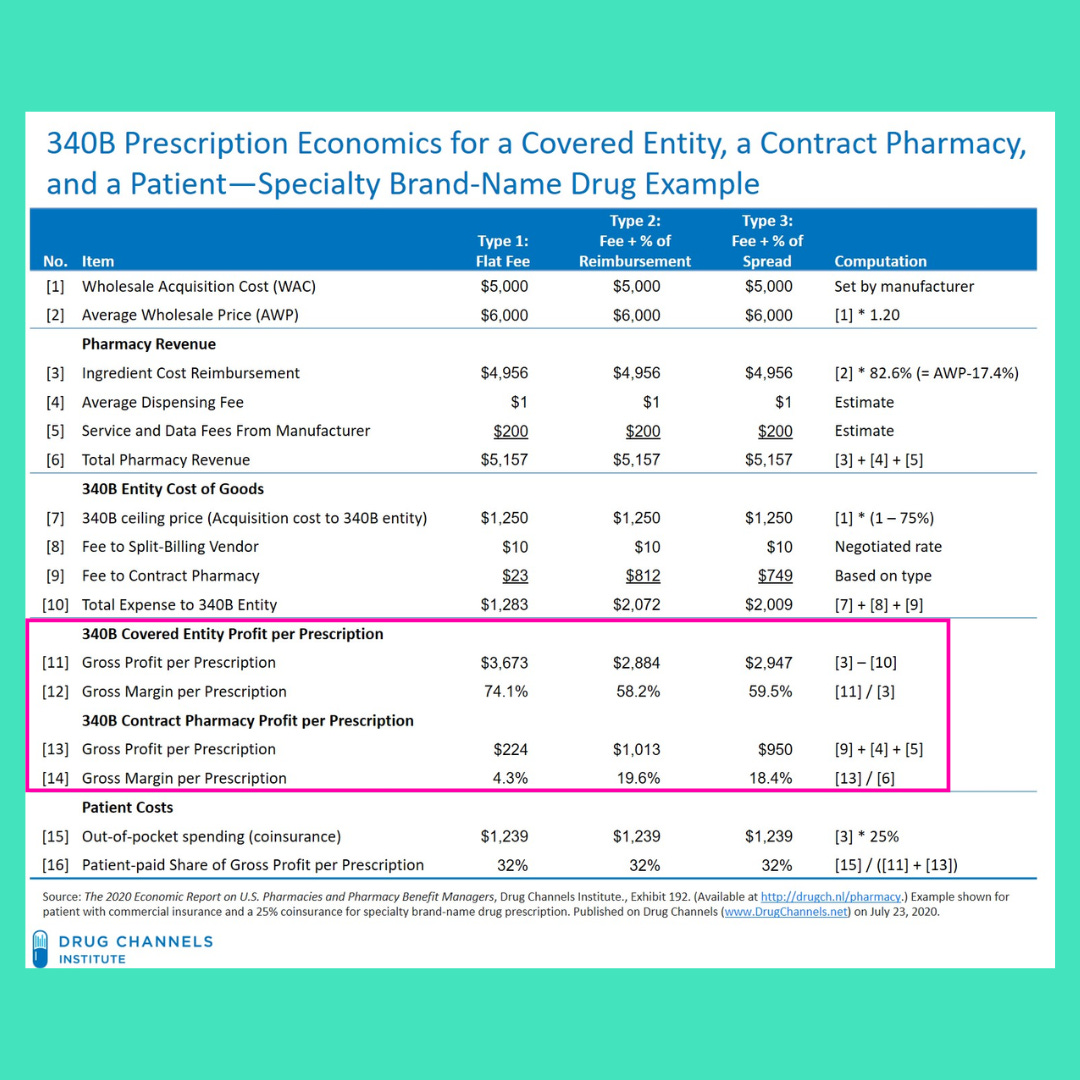
Here’s one more example from the master of pharmacy himself, Adam Fein on how much profit a hospital and a contract pharmacy stand to make through this program:
Herein lies the crux of the issue. Consolidation is afoot in healthcare. Mega systems are getting super mega. And when a rich af health system buys a small little community guy, they also buy access to the 340B program. That allows them to open clinics as extensions of the little community guy and give rich white people expensive drugs that the hospital bought at a discount, but reimbursed at the full amount, then pocket the profit.
See, now that the hospital can buy drugs at half price, doesn’t mean that a patient gets the drug at half price. The plan still reimburses the full amount of the drug. The PBM takes its cut. The contract pharmacy its cut. And the hospital gets the rest. The patient and the plan still pay the full reimbursement amount.
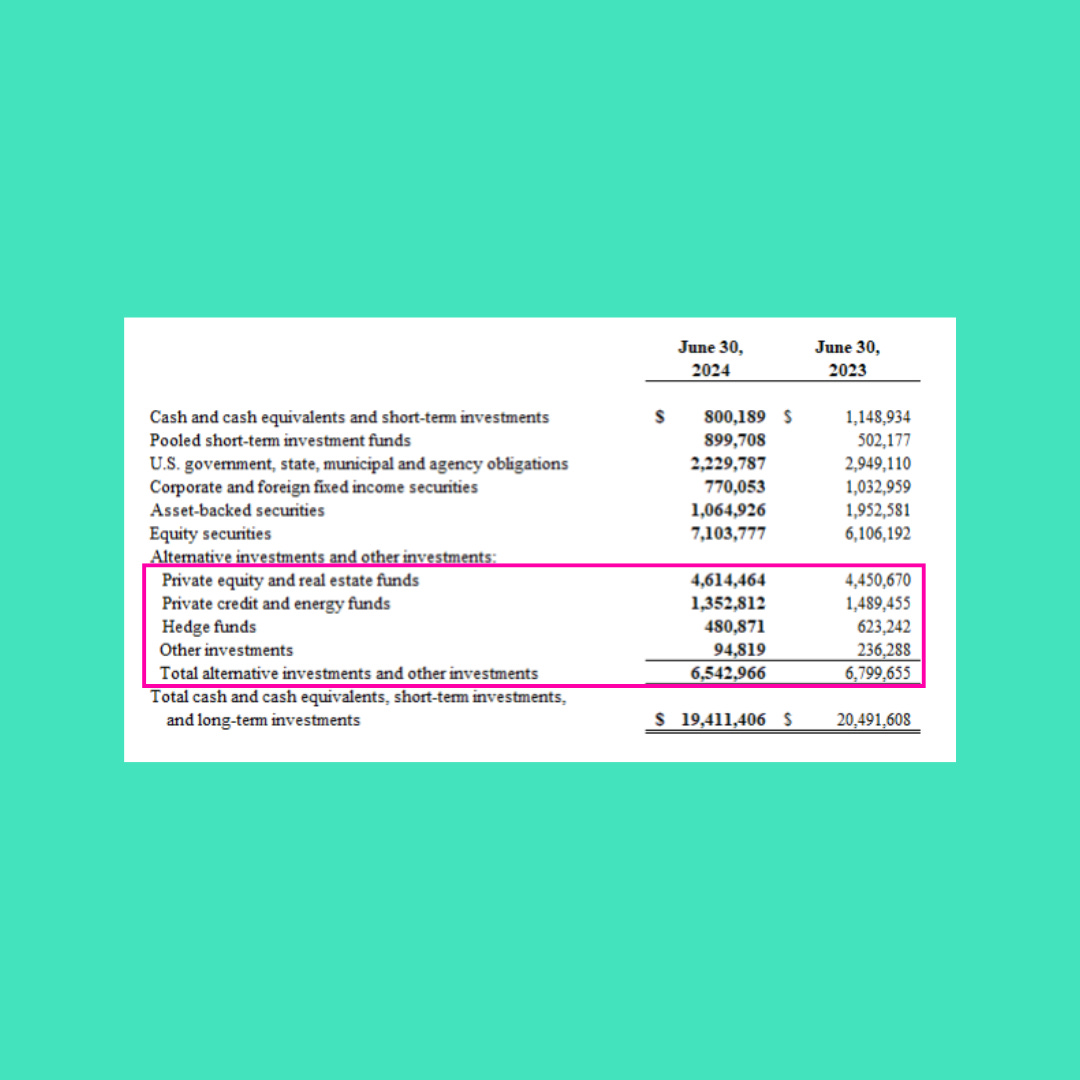
And if I sound a little salty this week, well, sorry not sorry. We’re talking about entities making billions of dollars, invested in private equity, hedge funds, and venture capital, stashing money in Venezuela and The Caymans, flying private jets around the world, opening hospitals in Dubai, while closing them in inner cities, all while taking advantage of the very people they supposedly are on a mission to save.
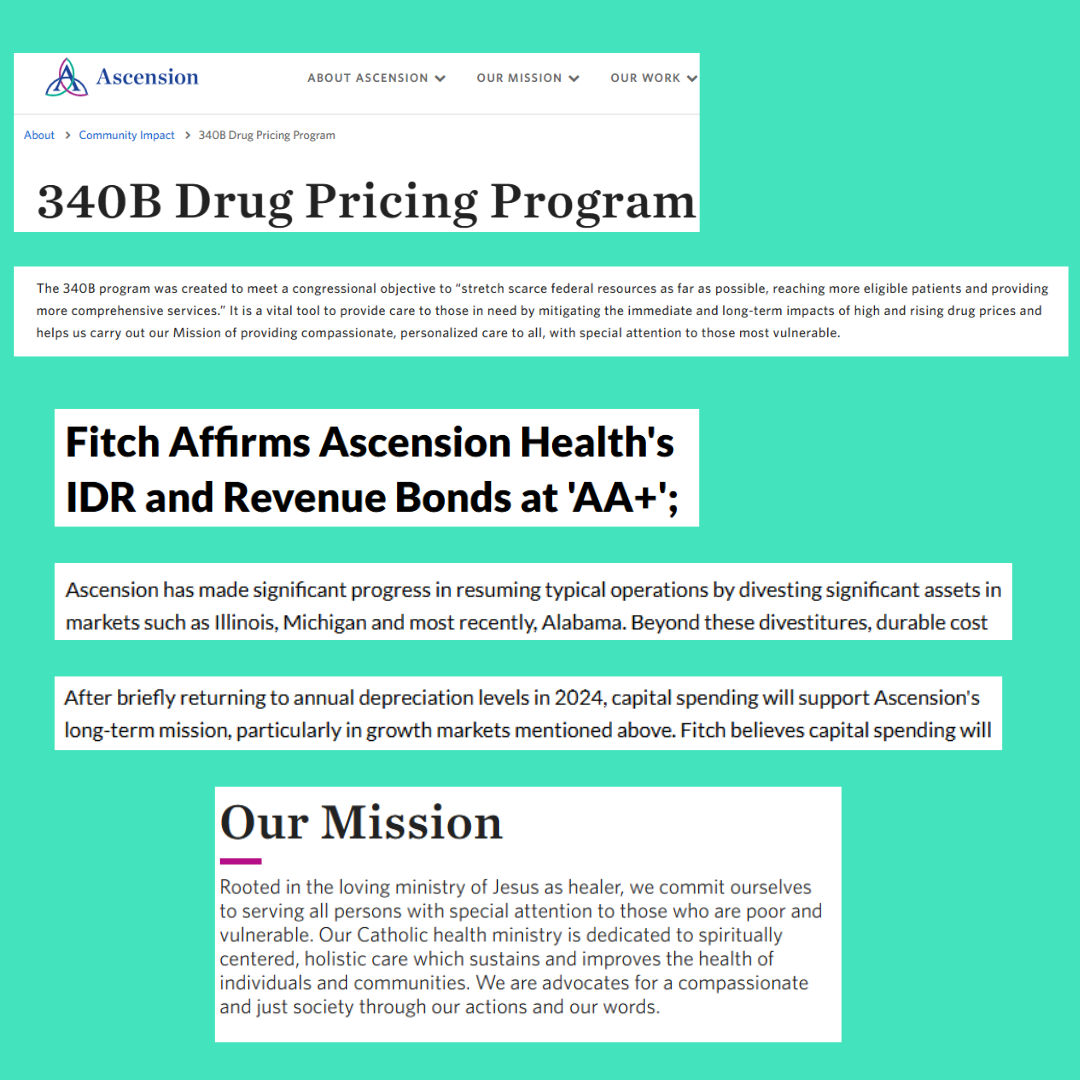
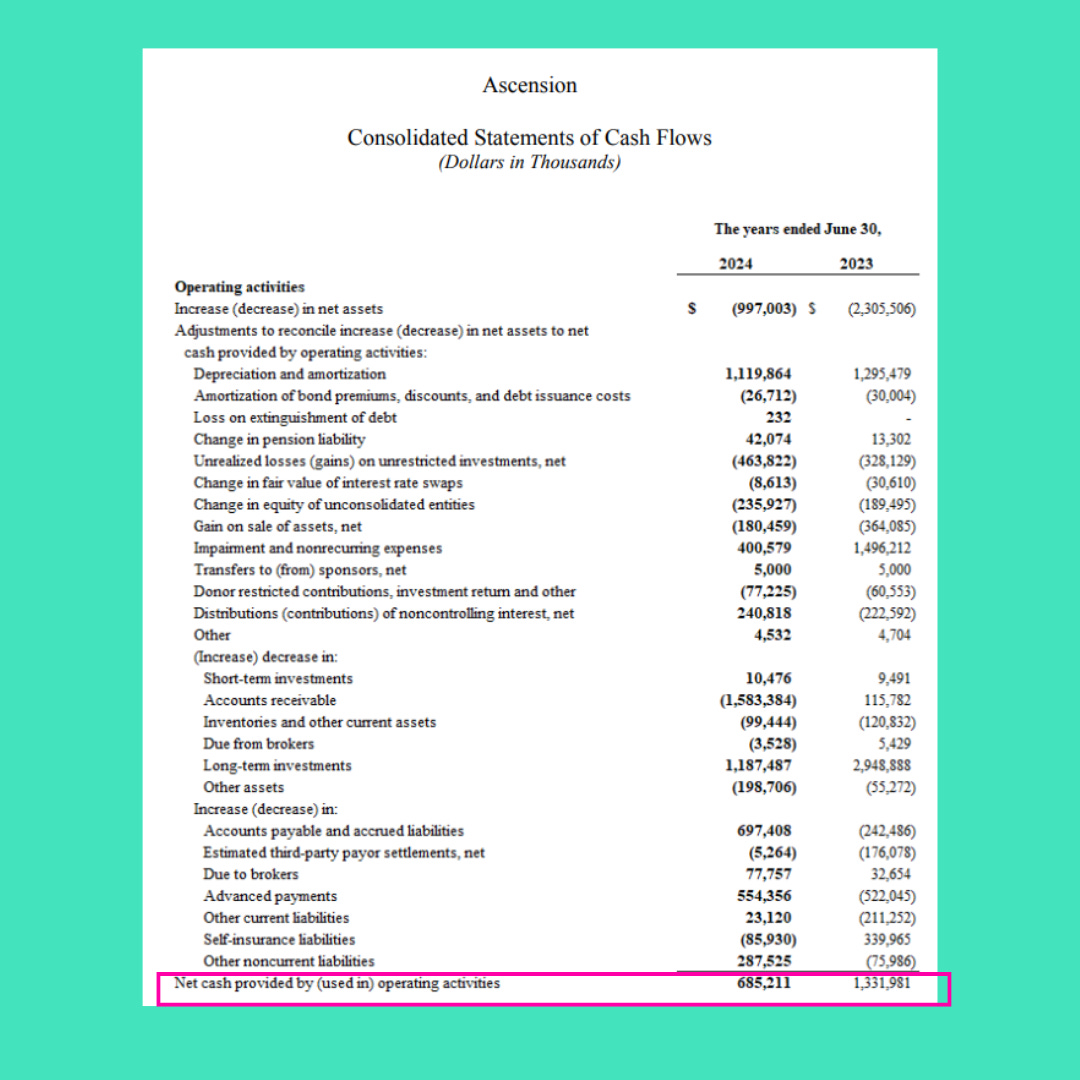
But don’t take it from me, take it from the wolf’s mouth:
And that $685M in cash is with an insane $1.5B increase in A/R from their own and Change Healthcare’s cyber attacks.
The loving ministry of Jesus Christ, serving Private Equity with billions of dollars while divesting in low-income markets. Pretty sure that’s what he would have done.
Also, this is one hospital. Now, extrapolate across all the large mega systems in the US. Yes, even Cleveland Clinic. 340B is definitely keeping them afloat. Or they are for sure passing on those savings to patients… ya…
Ok, I’m going to eat some ice cream not to get this salty taste out of my mouth.
Feel the Rhythm!


I think you are missing the mark here. The 340B program subsidizes not for profit urban/rural hospitals cancer/infusion service lines. Also, not all drugs are 340b eligible. In fact, I think you'd be surprised at what drugs are not 340b eligible. Every day the drug manufacturers remove more and more drugs from 340b eligibility.
An overwhelming majority of cancer patients are over the age of 65 (Medicare Reimbursement is the driver). The barometer for any business, especially an oncology/infusion treatment center is that the drug cost must be less than the Medicare Reimbursement for that drug. One of the most highly utilized drugs right now for cancer patients is Keytruda. Keytruda is NOT 340b eligible. Magically, it costs just under the reimbursement that Medicare pays. Also consider the ever-growing popularity of the Medicare Replacement plans that cater to patients on a fixed income. They are marketed as the same as Medicare for less. They cost those on Medicare less each month...until they use it and the Medicare Replacements put a majority of the infusion treatment payment...on the individuals on a fixed income and a lot of them do not pay their co-pay/deductible....but no cancer ever turns away a cancer patient who's in treatment because they're in bad debt status. Oh, and the previous few sentences assume that the insurance companies don't pull any of their denial tricks either...and I think you know a thing or two about that.
340b programs with their deep discounts offset these breakeven/loss patients/drugs. Look at Remicade. It's used for several treatments, particularly Crohn's disease. What makes Remicade particularly fascinating is that it's considered an Orphan drug in the eyes of 340b. Meaning that Critical Access Hospitals (who are automatically in 340b) do not get the 340b discounts attributed to this drug but the big urban/rural 340b eligible hospitals do get the discount. Last time I looked a few years ago, Remicade cost on average approximately $600 per infusion for a 340b hospital with Medicare reimbursement around $5,000. Great deal, right? Remicade cost Critical Access Hospitals, For Profit Hospitals and non 340b hospitals $5,500, with Medicare Reimbursement at $5,000. So guess what happens once hospitals realize this? No more Remicade infusions and patients now have to go elsewhere. If the overall mix of drug cost (via GPO pricing, etc.) is more than organizations receive in reimbursement, health systems are forced to have a hard discussion about cancer/infusion services. Many smaller hospitals across the country have stopped offering these services all together....but no one really talks about that do they?
Aside from this there's also several conversations being had today connecting the dots between Average Sales Price (ASP), pharmacy PBMs and Rebates from drug manufacturers. If you peel back this onion, I think you'll find a much better reason behind the skyrocketing drug prices.
Thanks for the shout out, Preston!